Description of the clinical case
The 4-year-old female child was referred to our hospital from a Ministry of Health Hospital at the age of three. She presented with delayed psychomotor development and irritability. She was diagnosed with WBS, Karyotype 46, XX. Physical examination revealed facial dysmorphia characterized by a broad forehead, short and wide nose, slight palpebral and epicanthal obliquity, a small jaw, and prominent lips. A systolic murmur of intensity IV/VI with a rhomboid characteristic (crescendo-decrescendo) and irradiation to the neck was observed in the aortic focus. The echocardiogram showed flow acceleration at the level of the aortic supravalvular junction.
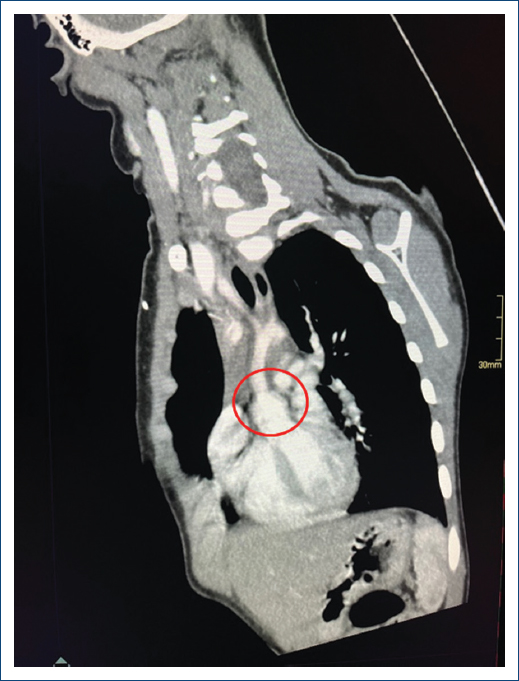
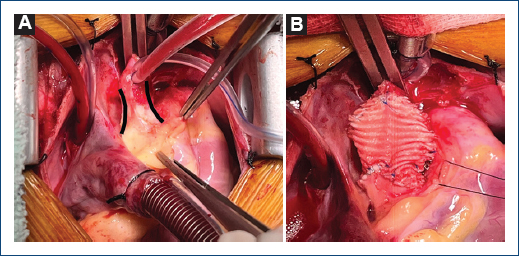
Complementary studies included a chest X-ray that revealed excavation of the lung button (Fig. 1) with no other relevant findings. The electrocardiogram showed ST depression, left ventricular growth with a positive Sokolow-Lyon index, suggesting signs of systolic overload and myocardial ischemia. The two-dimensional transthoracic echocardiogram confirmed concentric left ventricular hypertrophy; normal mobility; preserved ejection fraction of 70%; tri-leaflet aortic valve without alterations; the presence of severe SVAS with a maximum gradient of 116 mmHg and a mean gradient of 65 mmHg. The aortic annulus measured 10 mm (z-score-1.7); the sinuses of the Valsalva measured 14mm (z-score –1.3); and STJ measured 8 mm (z-score –3.6) (Fig. 2). These findings were confirmed with chest angiotomography (Fig. 3). Based on these findings, the diagnosis of SVAS was confirmed, and the decision was made to perform Doty’s procedure to resolve the stenosis. The girl is currently asymptomatic with regular cardiovascular follow-ups every 6 months.
Figure 1. Posteroanterior chest radiograph with a normal cardiothoracic index and button excavation pulmonar.
Figure 2. Two-dimensional transthoracic echocardiogram, A: parasternal long axis shows supravalvular aortic stenosis (red arrow), B: Doppler echocardiogram shows flow acceleration at the level of the STJ (black arrow) of 5.40 m/s.
Figure 3. Chest angiotomography, orthogonal and long-axis plane of the aortic roof, demonstrating the typical hourglass image (red circle), with an annulus of 17 mm (z 0.38) and an STJ of 8.8mm (z-3.6).